How to manage Malaria

Cause
Malaria is carried by thee female Anopheles mosquito and infection occurs following a mosquito bite and the injection of the insect’s saliva containing the malaria parasite into the wound. The disease occurs in many parts of the world and is caused by a parasite called Plasmodium. There are four species of Plasmodium, the most dangerous of these being Plasmodium falciparum.
Presentation
Malaria usually presents initially with flu-like symptoms: headaches, muscle and joint aches, and fever. Severe shivering attacks (rigors) and high fever then occur and recur in a cyclical pattern every third or fourth day. In severe cases of Plasmodium falciparum malaria, the urine may become bloody (blackwater fever) or the brain may be affected with unconsciousness and convulsions (cerebral malaria).
Prevention
No drug provides 100% cover against malarial infection. Prophylaxis must involve both mosquito avoidance and antimalarial drugs. Mosquito avoidance involves:
Antimalarial drugs
The drug of choice depends on the area visited, the presence or absence of drug-resistant P. falciparum malaria, personal allergies and idiosyncrasies to antimalarial medication, drug interaction with any maintenance medication a diver may be using, pregnancy, age, health and the availability of the drug. Consult your doctor to determine the best choice of medication and to ensure that no untoward side effects or contraindications are present.
Chloroquine 150 mg tablet: In South Africa, with the exception of the Ingwavuma and Ubombo districts, all species of malaria are, to date, chloroquine sensitive. Preventative treatment should begin 24 hours before entering an endemic area. In adults and children over 12 years, two tablets are taken initially, repeated weekly on the same day while in the area, and then weekly for four weeks after leaving the area. Children aged six to 12 years take one tablet; aged one to five years take half a tablet (or 10 m syrup); aged six weeks to 12 months take 5 m syrup.
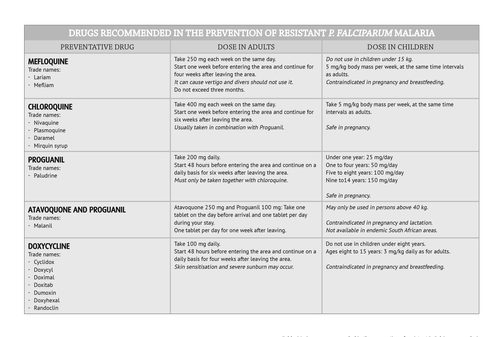
In areas where drug-resistant P. falciparum prevails (South-East Asia including Philippines, Thailand, Burma and China; Gabon and most of sub-Saharan Africa including the Comores and Madagascar; Sodwana; and the Ingwavuma and Ubombo districts of South Africa),
other antimalarial drugs are required.
Malaria is carried by thee female Anopheles mosquito and infection occurs following a mosquito bite and the injection of the insect’s saliva containing the malaria parasite into the wound. The disease occurs in many parts of the world and is caused by a parasite called Plasmodium. There are four species of Plasmodium, the most dangerous of these being Plasmodium falciparum.
Presentation
Malaria usually presents initially with flu-like symptoms: headaches, muscle and joint aches, and fever. Severe shivering attacks (rigors) and high fever then occur and recur in a cyclical pattern every third or fourth day. In severe cases of Plasmodium falciparum malaria, the urine may become bloody (blackwater fever) or the brain may be affected with unconsciousness and convulsions (cerebral malaria).
Prevention
No drug provides 100% cover against malarial infection. Prophylaxis must involve both mosquito avoidance and antimalarial drugs. Mosquito avoidance involves:
- meticulous application of insect repellent to exposed skin and clothing. The repellent of choice is N,N-diethyltoluamide (e.g. Peaceful Sleep, Mylol and Tabard lotions and sticks)
- wearing long-sleeved shirts or blouses, slacks and socks between sunset and sunrise (the feeding time of the Anopheles mosquito)
- moving continuously when outdoors at night (mosquitoes prefer a static meal)
- mosquito screening on all doors and windows
- spraying insecticide inside living quarters every day at dusk
- burning insecticide coils in the sleeping quarters at night
- sleeping under insecticide-impregnated mosquito nets tucked under the mattress.
Antimalarial drugs
The drug of choice depends on the area visited, the presence or absence of drug-resistant P. falciparum malaria, personal allergies and idiosyncrasies to antimalarial medication, drug interaction with any maintenance medication a diver may be using, pregnancy, age, health and the availability of the drug. Consult your doctor to determine the best choice of medication and to ensure that no untoward side effects or contraindications are present.
Chloroquine 150 mg tablet: In South Africa, with the exception of the Ingwavuma and Ubombo districts, all species of malaria are, to date, chloroquine sensitive. Preventative treatment should begin 24 hours before entering an endemic area. In adults and children over 12 years, two tablets are taken initially, repeated weekly on the same day while in the area, and then weekly for four weeks after leaving the area. Children aged six to 12 years take one tablet; aged one to five years take half a tablet (or 10 m syrup); aged six weeks to 12 months take 5 m syrup.
In areas where drug-resistant P. falciparum prevails (South-East Asia including Philippines, Thailand, Burma and China; Gabon and most of sub-Saharan Africa including the Comores and Madagascar; Sodwana; and the Ingwavuma and Ubombo districts of South Africa),
other antimalarial drugs are required.

Treatment
If malaria is suspected and there is absolutely no professional help available use:
Children of 10-15 kg: one tablet initially, repeat after eight hours; thereafter one tablet twice a day for the following two days (total: six tablets). Children of 15-25 kg: initially two tablets as a single dose; repeat two tablets after eight hours and thereafter two tablets twice a day for the following two days (total: 12 tablets).
Children of 25-35 kg: initially three tablets as a single dose, repeated after eight hours; thereafter three tablets twice a day for the following two days (total: 18 tablets).
Persons of 35-65 kg: initially four tablets as a single dose, repeated after eight hours; thereafter four tablets twice a day for the following two days (total: 24 tablets).
For persons over 65 kg, the same dose (total: 24 tablets) is recommended.
With new or recrudescent infections, a second course is recommended.
NOTE:
- A doctor must always be consulted, if at all possible.
- Self-treatment of malaria: Divers in remote malarial areas and without access to immediate medical treatment may be faced with the problem of an unexplained fever, headache, body aching and rigors. Self-treatment is potentially very dangerous.
If malaria is suspected and there is absolutely no professional help available use:
- Coartem (artemether 20 mg, lumefantrine 120 mg) tablets. Take with food/fluids. Repeat dose if vomiting occurs within one hour of administration. An intensive three-day course is recommended. The dose depends on body mass.
Children of 10-15 kg: one tablet initially, repeat after eight hours; thereafter one tablet twice a day for the following two days (total: six tablets). Children of 15-25 kg: initially two tablets as a single dose; repeat two tablets after eight hours and thereafter two tablets twice a day for the following two days (total: 12 tablets).
Children of 25-35 kg: initially three tablets as a single dose, repeated after eight hours; thereafter three tablets twice a day for the following two days (total: 18 tablets).
Persons of 35-65 kg: initially four tablets as a single dose, repeated after eight hours; thereafter four tablets twice a day for the following two days (total: 24 tablets).
For persons over 65 kg, the same dose (total: 24 tablets) is recommended.
With new or recrudescent infections, a second course is recommended.
- Fansidar (pyrimethamine/sulphadoxine) as a single dose (three tablets for adults, two tablets for ages nine to 14, one tablet for ages four to eight; half a tablet for ages under four).
NOTE:
- Coartem and Fansidar are temporary measures only and a doctor must then be found and consulted urgently.
- Safety in pregnancy and lactation has not been established. Side effects have been reported and special precautions do exist. If at all possible, contact a doctor before using the treatment.
Posted in Dive Safety FAQ, Dive Safety Tips
Posted in Malaria, Dive Travel, Out and about, diver in distress, medications
Posted in Malaria, Dive Travel, Out and about, diver in distress, medications
Categories
2025
2024
February
March
April
May
October
My name is Rosanne… DAN was there for me?My name is Pam… DAN was there for me?My name is Nadia… DAN was there for me?My name is Morgan… DAN was there for me?My name is Mark… DAN was there for me?My name is Julika… DAN was there for me?My name is James Lewis… DAN was there for me?My name is Jack… DAN was there for me?My name is Mrs. Du Toit… DAN was there for me?My name is Sean… DAN was there for me?My name is Clayton… DAN was there for me?My name is Claire… DAN was there for me?My name is Lauren… DAN was there for me?My name is Amos… DAN was there for me?My name is Kelly… DAN was there for me?Get to Know DAN Instructor: Mauro JijeGet to know DAN Instructor: Sinda da GraçaGet to know DAN Instructor: JP BarnardGet to know DAN instructor: Gregory DriesselGet to know DAN instructor Trainer: Christo van JaarsveldGet to Know DAN Instructor: Beto Vambiane
November
Get to know DAN Instructor: Dylan BowlesGet to know DAN instructor: Ryan CapazorioGet to know DAN Instructor: Tyrone LubbeGet to know DAN Instructor: Caitlyn MonahanScience Saves SharksSafety AngelsDiving Anilao with Adam SokolskiUnderstanding Dive Equipment RegulationsDiving With A PFOUnderwater NavigationFinding My PassionDiving Deep with DSLRDebunking Freediving MythsImmersion Pulmonary OedemaSwimmer's EarMEMBER PROFILE: RAY DALIOAdventure Auntie: Yvette OosthuizenClean Our OceansWhat to Look for in a Dive Boat
2023
January
March
Terrific Freedive ModeKaboom!....The Big Oxygen Safety IssueScuba Nudi ClothingThe Benefits of Being BaldDive into Freedive InstructionCape Marine Research and Diver DevelopmentThe Inhaca Ocean Alliance.“LIGHTS, Film, Action!”Demo DiversSpecial Forces DiverWhat Dive Computers Don\'t Know | PART 2Toughing It Out Is Dangerous
April
